By Dr Darren Weiss, Executive Director, HSF
Oral diseases and conditions – tooth decay (caries), gum disease (severe periodontitis) and tooth loss – affect 3.5 billion people worldwide. Untreated caries in adult teeth is the most prevalent of all medical conditions. Migraines come in second, and third place is held by periodontitis.
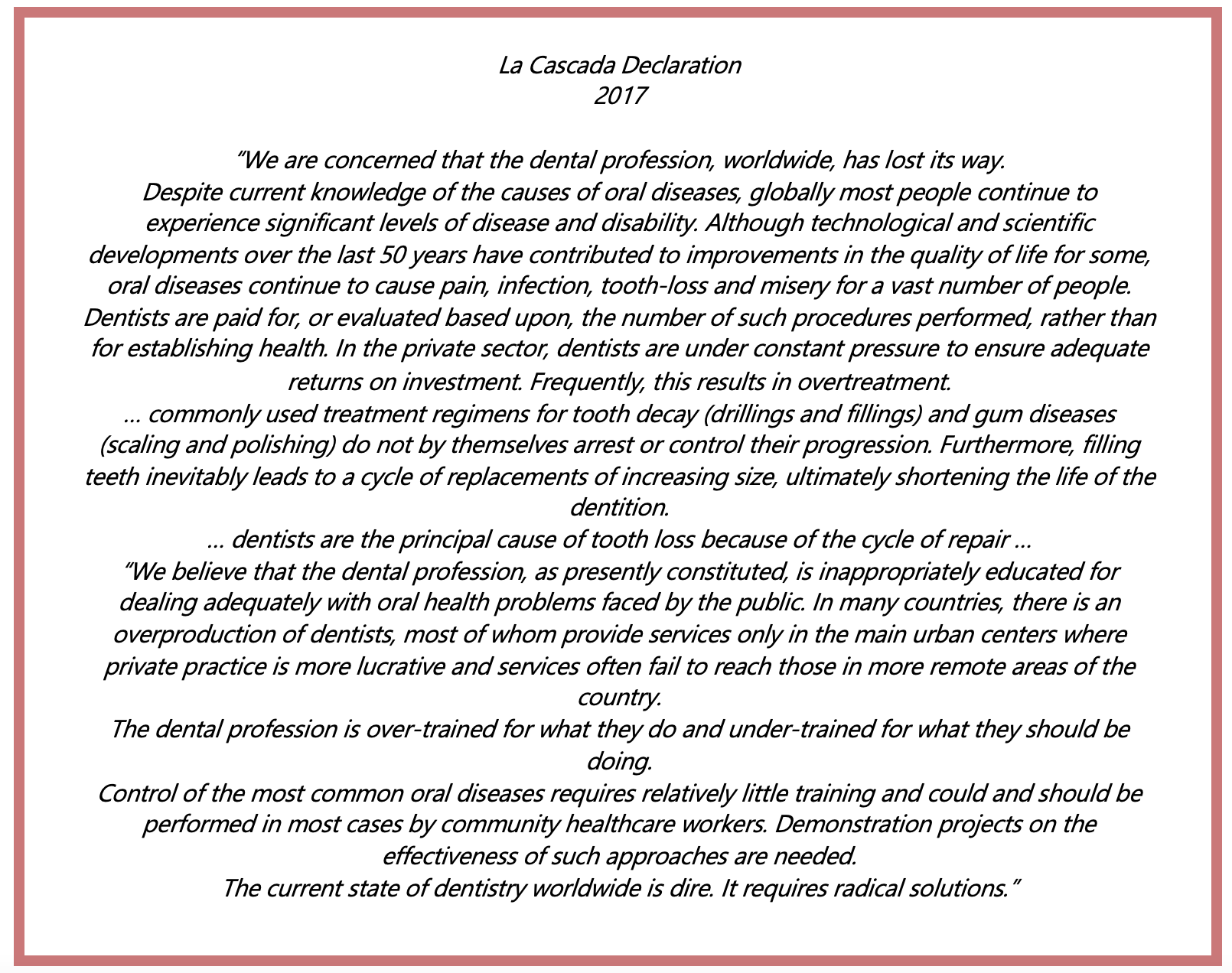
Dentistry has traditionally owned Oral Health Care (OHC). But now there is a growing recognition that dentistry has lost touch with the reality of the global oral disease burden. Framed are some quotes from the La Cascada Declaration made by leading OH global experts in 2017.
This is because OHC is simply not deployed in the right places. Oral Health professionals and resources are not appropriated according to needs or disease distribution. OHC sprouts up wherever there is a return on investment.
So dentistry has largely been unable to combat the global challenge of oral diseases. This shortcoming is not the fault of individual dental clinicians committed to caring for their patients. The overall dental surgeon paradigm, system, and model of dental care delivery are at fault.
In high-income countries, the current reactive, treatment-dominated, increasingly high-tech, interventionist, and specialised approach, that reflects the surgical origins of the profession, is not tackling the underlying causes of disease and is not addressing inequalities in oral health. In low-income and middle-income countries, the limitations of so-called westernised dentistry are at their most acute; dentistry is often unavailable, unaffordable, and inappropriate, particularly for the rural poor.
Of all the health services, OHC is the least integrated into primary care. Of all the Non-Communicable Diseases (NCDs), Oral Health (OH) is the least integrated into the NCD prevention agendas.
As oral diseases and conditions share common risk factors with other NCDs, the consolidation of preventive interventions and activities around those risk factors may very well be the way forward for OHC. It may not look like dentistry – but we all know where dentistry got us.
Prevention of NCDs by addressing their causes will become best practice because dealing with the consequences of NCDs is costly for the healthcare provider as well as for the patients. As the pathology or physiological changes associated with NCDs are largely irreversible, patients pay the price for lack of prevention with their quality of life. Therapeutical practices such as surgery, are sadly often too late for people who want to get the most out of life.
The day will come when Community Health Workers (CHWs) or Health Promoters (HPs) trained in Oral Health Promotion (OHP) will share the frontlines of primary care with doctors and nurses. They will indeed change the very nature of the frontline. Health Promoters will come from, and operate, within the community. Their familiarity and agility will enable access to primary care everywhere, even in remote villages. They will have digital tools based on artificial intelligence to liaise with health specialists, to diagnose and triage conditions, and to survey the health status of the community. They will be trained to comprehend simple didactic preventive messages, such as no smoking, exercise daily or no added sugar. But the HPs will deliver those messages in a way the community will best understand and accept them. There needs to be a career-track in place for CWS/ HPs to develop their knowledge and skills, and take on more responsibility.
What will the OHC providers do? What will become of the dentists?
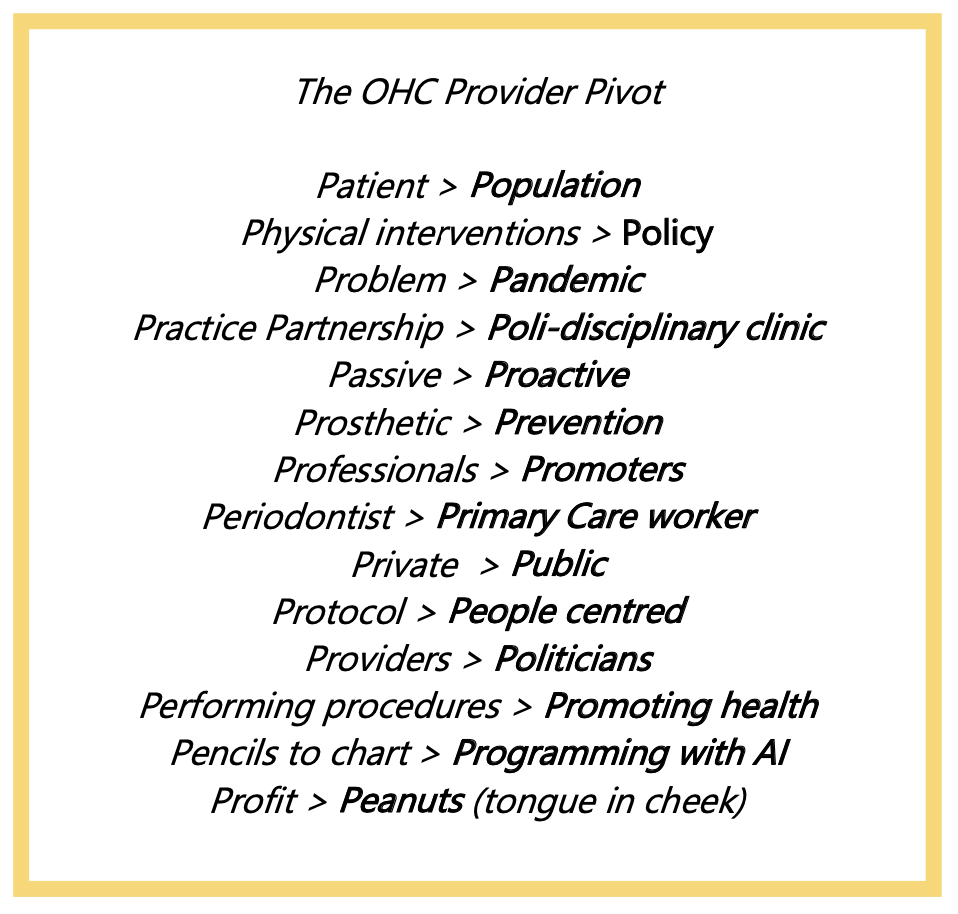
The best clinicians will continue to drill and fill teeth just like their specialist colleagues who are managing and restoring soft and hard tissue issues, correcting bites, aligning crowded teeth and beautifying smiles. Those who want to be part of the solution for the inequity and burden of global oral disease, or wish to realign with global disease distribution, will have to transition. In a play of words starting with the letter P, framed are 14 ways in which the OHC provider will need to Pivot:
Where are we transitioning to?
If dental care has been busy with managing proximal determinants of oral diseases such as biological and behavioural factors (like infection, hygiene and diet); then greater impact of interventions can be found upstream with social, commercial and environmental circumstances (such as socioeconomics and corporate marketing). And there are opportunities even further upstream such as advocacy for improved policies and regulations (like they did with smoking). Hence, like anadromous fish such as salmon, OHC will transition up-stream.
Recently the WHO has called for OHC to align and integrate with programs for prevention & control of NCDs & Universal Health Coverage as well as environmentally friendly & less invasive dentistry. Mobile technologies for health interventions are being encouraged, and 3 forms of professional fluoride delivery have been added to the WHO list of essential medicines.
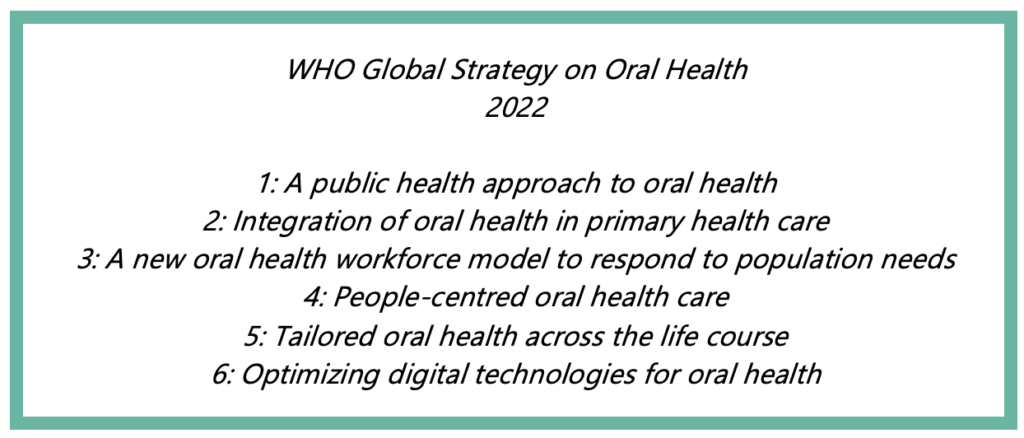
Most recently, the WHO published its Global Strategy on Oral Health – the 6 guiding principles in the frame are worth noting:
The Corona pandemic has shaken-up our awareness of disease determinants and exposed a truth that NCDs (and Corona) cluster within social groups according to patterns of inequality deeply embedded in our societies. A key to recovering stronger from the pandemic is to keep populations in better health, by ensuring that NCDs are more effectively prevented, diagnosed, managed, and treated. This includes addressing poverty and inequalities, barriers to accessing quality healthcare, and the preventable harm caused by tobacco, alcohol, ultra-processed food and drinks, and pollution.
The day will come when caries, alongside diabetes, obesity, heart and lung disease and other NCDs, will be addressed in primary care based on their common disease determining factors – even if it means starting to swim like salmon against the current.